Bedaquiline combined with other active drugs has the potential to achieve high culture conversion rates in advanced MDR- and XDR-TB cases. However, it is crucial to follow carefully all patients for severe adverse events, even after bedaquiline discontinuation.
Use of the new anti-tuberculosis (TB) drug bedaquiline as part of a tailored regimen achieved high rates of culture conversion in people with multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB), French investigators report in the online edition of Clinical Infectious Diseases.
The study population comprised 35 people who were provided with compassionate access to the drug between 2011 and 2013. After six months of therapy, 97% of study participants with culture-positive pulmonary TB at baseline had achieved culture conversion. The overall safety profile of the drug was satisfactory, but two people discontinued therapy because of a potentially dangerous disturbance in their heart rhythm.
The World Health Organization (WHO) estimates there were 450,000 new cases of MDR-TB (TB with resistance to the first-line drugs isoniazid and rifampicin) in 2011. An estimated 10% of MDR-TB cases also involve resistance to second-line agents, and cases with resistance to fluoroquinolones and injectable drugs are defined as XDR-TB.
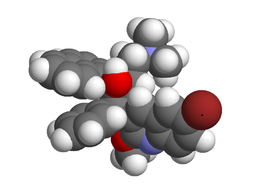
Bedaquiline is a new antibiotic with activity against drug-resistant strains of TB. It was approved by the Food and Drug Administration (FDA) in the United States and the European Medicines Agency after it demonstrated efficacy in clinical studies.
Investigators in France wished to further evaluate the efficacy, tolerability and safety of bedaquiline. They therefore performed a retrospective analysis of six-month outcomes in 35 people with MDR-TB and XDR-TB who were provided with compassionate access to the drug.
Bedaquiline was combined with a median of four other anti-TB agents selected after drug susceptibility testing. People with pulmonary TB had regular smear and culture examinations throughout follow-up. Other evaluations included monitoring of liver function (ALT and AST) and ECG examinations to monitor heart rhythm, especially prolongation of QT interval (60ms increase or above).
The study participants had a median age of 39 years. Only one was born in France. None had HIV co-infection, but half had hepatitis C virus (HCV) infection.
All but one of the participants (97%) had pulmonary TB, including five (14%) with extra-pulmonary involvement.
Of the participants with pulmonary TB, 76% had the infection in both lungs, 85% had at least one lung cavity and 85% were sputum-smear positive at baseline.
Of the 29 people with culture-positive TB at baseline, 72% achieved culture conversion after three months of therapy and 97% after six months.
The authors note that the efficacy was better than that observed in clinical trials.
Sputum-smear conversion occurred in 48% and 69% of participants at three and six months, respectively.
The median time to culture conversion was 85 days.
Therapy with a regimen containing a fluoroquinolone was associated with culture conversion (p = 0.001). In contrast, the presence of lung cavities (p < 0.001) and HCV infection (p = 0.001) were both associated with slower time to culture conversion.
There was one death. This was due to throat cancer and was not related to either TB or bedaquiline therapy.
Mild elevations in liver enzymes were observed in five people (14%), with more severe increases in an additional two individuals (6%). However, these two patients were also taking other agents with potential liver toxicity.
ECG evaluations showed that mean QT interval increased by a median of 1.96ms during therapy. An increase in QT interval of 60ms or greater was observed in seven individuals (20%), and three (9%) had an increases above 500ms. Persistent increases in QT interval caused the discontinuation of bedaquiline in two people.
The authors were encouraged by their findings, which they suggest show that bedaquiline “combined with other active drugs has the potential to achieve high culture conversion rates in advanced MDR- and XDR-TB cases.” However, they caution, “it is crucial to follow carefully all patients for severe adverse events, even after bedaquiline discontinuation.”
Reference
Guglielmetti L et al. Compassionate use of bedaquiline for the treatment of MDR- and XDR-tuberculosis: an interim analysis of a French cohort. Clin Infect Dis, online edition, 2014.
Source: Aidsmap